
4. JPEF 2019: Award Winning Abstract 2
This research paper was awarded the second position in the best paper award category at the 7th JPEF Annual Global Diabetes Convention 2019.
PREVALENCE OF INSULIN RESISTANCE IN NON-OBESE, EUGLYCEMIC AND NORMOTENSIVE FIRST DEGREE RELATIVES OF OBESE INDIVIDUALS
Nishanth Dev1, Jhuma Sankar2
1 Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India
2 All India Institute of Medical Sciences, New Delhi, India
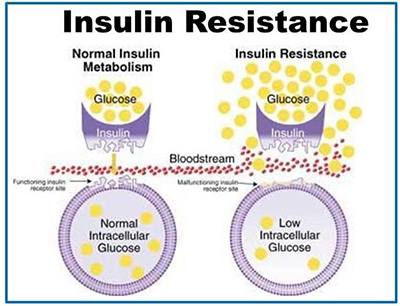
Background & Aim: Insulin resistance (IR) is an important etiology for development of prediabetes and type-2 diabetes. While most studies have focused on the prevalence of IR in obese, diabetics and hypertensive individuals, there is scarcity of literature on the first-degree relatives of these populations. The study was undertaken to estimate the prevalence of IR in Normotensive, euglycemic, non-obese first- degree relatives of obese individuals.
Material & Methods: This cross-sectional study included 35 first degree non-obese, euglycemic and normotensive relatives of obese individuals compared with 35 matched first degree relatives of non-obese individuals. The enrolled individuals were subjected to history, clinical examination and investigations. Insulin resistance was defined as Homeostasis model assessment-estimated insulin resistance (HOMA IR)value exceeding the 75th percentile of the total study group.
Results: The prevalence (95% CI) of insulin resistance was 34% (21 to 51) in the study group as compared to 14% (6 to 9%) in the comparison group (p=0.05), (Odds ratio (OR) 95% CI: 2.4 (0.94 to 6.09). The corresponding mean HOMA IR levels were 2.5 and 2.2 respectively. Impaired fasting glucose levels were seen in 26% in study group as compared to 11% in the comparison group (OR: 2.25 (0.76 to 6.62)). Higher proportions of subjects in the study group had impaired glucose tolerance compared to the comparison group (23% vs. 9%; OR: 2.67 (0.77 to 9.23)). The mean fasting as well as post-prandial glucose levels were higher in those with IR as compared to those without (98 vs. 88, p=0.002 and 128 vs. 121, p=0.05 respectively). All individuals with IR had increased serum insulin levels and the corresponding meanserum insulin levels were 184 as compared to 114 in those without IR (p <0.0001). The differences in lipid parameters were not statistically significant between the groups.
Conclusion: The study demonstrates significant burden of Insulin resistance in healthy relatives of obese individuals and should be closely followed up and monitored so that early interventions by means of life style and diet modifications can be done. Our findings are hypothesis generating and exploratory which needs further confirmation by larger studies.
For enquiries info@jothydev.net.
Please visit: jothydev.net | research.jothydev.com | diabscreenkerala.net | jothydev.com/newsletter
