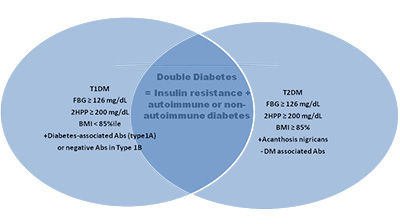
3. Double or Hybrid Diabetes
Diabetes is considered as a global epidemic that affects the life of millions
of people. While type 1 diabetes (T1D) is caused by autoimmune destruction of
the insulin-producing beta cells of the pancreas, type 2 diabetes (T2D) results
from a combination of insulin resistance and beta cell insulin secretory defect.
One recent finding reports the incidence of a new type of diabetes namely
double or hybrid diabetes (DD) that demonstrates symptoms of both T1D and T2D.
An article published on Nature’s Nutrition & Diabetes discussed the worldwide
prevalence of DD, its main physiological characteristics including beta-cell
autoimmunity, insulin resistance, cardiovascular disease, and the main risk
factors of developing DD.
The term ’double diabetes’ refers to the incidences where the patient demonstrates characteristics of both T1D and T2D. Common symptoms of DD include obesity, insulin resistance, type of latent autoimmune diabetes in youth (LADY), presence of GAD56, IA2 autoantibodies and insulin antibodies in T1D. DD can be a major event during the young onset (11–19 years old) of patients with diabetes due to weight gain and insulin resistance resulted as side effects of insulin treatment. Potentially positive family history and increased BMI (>85th percentile) could be considered as clinical measures to recognize such DD cases from those with visible T1D. DD phenotype must be appropriately managed in terms of both the diagnosis and therapeutic approach as it is extremely hard for these patients, who are usually mainly identified during paediatric ages. DD appears to be an independent and potential risk factor for patients with T1D in gaining macro and microvascular diseases. Microvascular diseases in DD will be an elevated risk for nephropathy and retinopathy, while macrovascular comorbidities include the metabolic syndrome.
The incidence of DD was reported in 1991 by the observation that insulin deficiency and insulin resistance co-exists. The first epidemiological data along with heredity observations made clinicians estimate that around 4% of all T1D patients have the possibility of T2D also along with T1D. With the increasing rate of obesity among children with T1D, approximately 25% suffered from excess body weight, which could be correlated with the symptoms of T2D such as poor diabetic control, unstable levels of blood glucose and elevated insulin dosages. More recently, in 2016 one study led by Merger et al also confirmed that among T1D patients, 25.5% exhibited higher macrovascular-associated comorbidities, such as coronary heart disease and stroke, increased microvascular conditions, both independently of glucose control. In another study including 200 patients with youth onset diabetes, 7% with the mean age of 22.2 years and mean BMI of 29.8 were categorized in DD, with 29% still under the unknown category.
Double Diabetes, should not be considered as a simple, single clinical entity, but comprises of a mixed range of complex pathophysiological disease features including impaired immunity, autoimmunity, Insulin resistance, and cardiovascular disease. The risk factors that may lead to complex disorders like DD include genetic, pathophysiological, environmental and lifestyle.
For enquiries info@jothydev.net.
Please visit: jothydev.net | research.jothydev.com | diabscreenkerala.net | jothydev.com/newsletter
